During the height of the coronavirus pandemic, elderly members of a synagogue in Cambridge, Massachusetts, decided to visit the Division of Infectious Diseases at Boston Children’s Hospital to donate their blood to science.
As part of the Precision Vaccines Programme, a research project that develops vaccines for vulnerable populations, their blood would be used to test the efficacy of vaccine adjuvants – substances that are added into vaccines alongside the active ingredient to enhance its effects on the body.
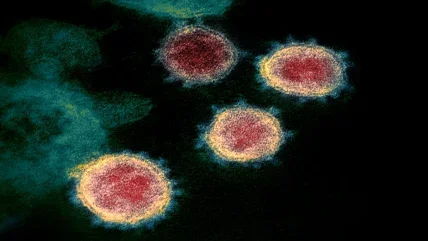
Adjuvants have been around since the 1920s, but most notable advances in the field have happened in recent decades. Now, as labs across the world work to develop better Covid-19 vaccines, adjuvants are in the spotlight once more. It’s easy to see why: they can make the effects of a vaccine last longer and provide a greater degree of immunity. In other words, with the right adjuvant, we could have a Covid vaccine that lasts years, rather than months, all while protecting us against multiple variants.
But while we have some understanding of how adjuvants work, we still don’t know exactly how we can use them to make vaccines more effective, says head of VFI-Oxford Adjuvant Programme at the Jenner Institute at Oxford University, Dr Anita Milicic. “It’s the million dollar question… [we need] increases in knowledge along the whole path of the immune response, from how the adjuvants activate our immune system in the first place to how it responds to a vaccine eventually. We’re trying to understand all of those steps.”
How close are we to realising the potential of adjuvants? While research is wide-ranging and ongoing, we can look to some promising areas of investigation for a sense of where the field is headed.
The guarantees
“We know that, generally speaking, adjuvants induce inflammation, they induce irritation of our biological systems, and those inflammatory processes then enhance the immune response to the vaccine that is given with the adjuvant,” says Dr Milicic. These processes work to mimic the body’s natural immune response, effectively tricking it into responding as if it had come into contact with a virus or bacteria.
Over the past few decades, we’ve learned more about how adjuvants can be used, including the 2011 Nobel-prize winning discovery that innate immunity (our body’s natural defence system) drives adaptive immunity (immunity that we acquire after being exposed to a disease). Toll-like receptors (TLRs), a class of proteins, were recognised as playing a crucial signalling role in this process, and several adjuvants that initiate a TLR response have since been approved for use in licenced products.
More adjuvants have been discovered in recent decades than in the past 80 years, with research spurred on by increased funding and institutional support in light of the pandemic. The NIH, for example, established adjuvant discovery and development programmes within its already-established consortiums, leveraging assets among public and private organisations to rapidly respond to the current, as well as future, pandemics.
The research process carried out on potential adjuvants must consider what type of immune response needs to be induced to protect against a certain disease, and then determine which substance or substances in combination can create that response, says Dr Milicic. “We need to join the dots between all those things to get a bigger, better picture.” Adjuvants that are currently approved for use include aluminium salts (Alum), certain oil-in-water emulsions, and types of saponins, a plant-derived compound.
The right combination
For each virus or bacteria, there could be multiple adjuvants that trigger the immune response when combined with an antigen, says Krishnendu Roy, professor and Robert A. Milton chair in the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University. And now, there’s increasing interest in how these can be combined in certain ways to create the desired or even a greater effect.
“We have tried single-agent vaccines for many years, in many things. But in diseases where either the virus or bacteria has figured out how to avoid the immune system, or the vaccine response hasn’t been strong, I think it’s absolutely rational to try combination adjuvants,” says Roy.
When adjuvants are combined, there are certain attributes that Dr Ofer Levy, Harvard Medical School professor, physician, and director of the Precision Vaccines Programme, and his team look for when evaluating the potential of the substance. “You could get additivity, antagonism, or synergy. We look for synergistic combinations and those interactions that are age-specific,” he says.
Synergistic combinations are when combined molecules produce a unique effect beyond being a simple summation of their individual effects (additive), and that is greater than if they were given alone.
We have tried single-agent vaccines for many years, in many things. But in diseases where either the virus or bacteria has figured out how to avoid the immune system, or the vaccine response hasn’t been strong, I think it’s absolutely rational to try combination adjuvants.”
Krishnendu Roy, Georgia Tech and Emory University
Once a substance is identified, it’s evaluated based on its efficacy and toxicity – the adjuvant needs to work well while also being safe to use, says Roy. However, the jury is still out on whether combination adjuvants are more effective across the board than single adjuvants, he adds.
So far, though, combination adjuvants have shown promise. The first combination adjuvant to be licenced was AS04 in 2005, developed by GlaxoSmithKline (GSK). It combines a TLR agonist with Alum and today is used in a HPV vaccine (Cervarix), which is highly effective against certain types of HPV. Could we soon see vaccines with similar efficacy in other therapy areas? Researchers are working on it. Many adjuvants are currently in clinical development for diseases such as tuberculosis, malaria, and the flu.
Delivery technology
Identifying an adjuvant is only part of the battle – how it behaves once it’s delivered into the body can determine how well the vaccine works, and what sort of side effects it creates. This is where delivery technology comes in. Adjuvants can be incorporated into lipid nanoparticles or other nano formulations or emulsions, and the formulation in which they are delivered can affect whether the right cells and tissue are being targeted without causing any systemic toxicity, says Derek O’Hagan, senior vaccines R&D advisor and GSK fellow at GSK.
“It’s a delivery challenge, to ensure that you’re getting the right activation signal in a controlled fashion, so you’re not going to trigger adverse effects because you’ve got too much activation of too many cells.”
“In the bigger picture perspective…it’s every bit as important as all the other sophisticated immunological cells. It’s what triggers, it’s what controls.”
Derek O’Hagan, GSK
GSK uses the concept of adjuvant systems (AS), a term they’ve coined, to create adjuvants whose formulation considers how they will be delivered into the body. AS04 is one such adjuvant, alongside others AS01 and AS03.
One success story is GSK’s Shingrix vaccine, which uses AS01 with a single glycoprotein, and from two doses offers 90% protection against shingles that stays above 85% for at least four years. As well as making them more effective, delivery technology can help to make vaccines safer, and this is the direction that the field is moving in, says Roy. “I think there will be a lot more adjuvants and combination adjuvants coming in with a better safety profile and that are packaged [within delivery technology].”
Roy has received funding from the NIH to screen and evaluate potential adjuvants for Covid vaccines, and considering how they could be delivered has been a key part of this work. For O’Hagan, formulation delivery is a crucial area of focus as the field advances. “It creates the adjuvant system that makes everything else happen,” he says. “In the bigger picture perspective…it’s every bit as important as all the other sophisticated immunological cells. It’s what triggers, it’s what controls.”
Focus on the future
The potential of adjuvants is immense. Not only could we have vaccines that are more effective, last longer, and have fewer side effects, but researchers have their sights set on huge global disease areas. “HIV, malaria, TB, and a universal flu vaccine are the big four we were trying to address before the pandemic,” says Dr Milicic of her work at the Jenner Institute. Now, Covid-19 is in the mix, too.
For Dr Levy, adjuvants hold huge potential in precision medicine, as different populations can react differently to the same formulation. “We’ve developed the techniques to allow us to accelerate and de-risk adjuvant development and to tailor the adjuvant, so it’s more suitable for a particular vulnerable population that you’re trying to protect,” he says.
Plus, thanks to the pandemic, getting a vaccine from the lab to the clinic might become easier, too. "When it comes to vaccines, the coronavirus pandemic has broadened our mindsets. Novel vaccine approaches and formulations, as long as they show good safety and efficacy, may become easier to gain regulatory approvals for the future,” says Dr Milicic. Ultimately, the potential of adjuvants lies in how well we can understand the science behind their mechanisms – and how we can use this knowledge to influence the immune system, says O’Hagan.
“Can we have what we call an adjuvant, which is a molecule that modulates the immune system, to do something completely different? What about where the immune system has not quite done what we want it to do, say by clearing cancer? Can we give the immune system a boost to help it do that? Maybe.”
The same could be true for a variety of therapy areas, including autoimmune diseases, chronic infectious diseases, or a situation where the immune system has gone awry, he adds. “Can we get in there and modulate it? I think this is the space that’s in front of us.”





